Earlier this year (19 January 2023), the United States reported its first two cases of gonorrhoeal infection that had a reduced likelihood of responding to antibiotics.
Even though gonorrhoeal infections are rarely life-threatening, this short post describes particular characteristics that enable Neisseria gonorrhoeae to be such a successful pathogen and explains why cases of multi-drug resistant gonorrhoea are a serious public health concern.
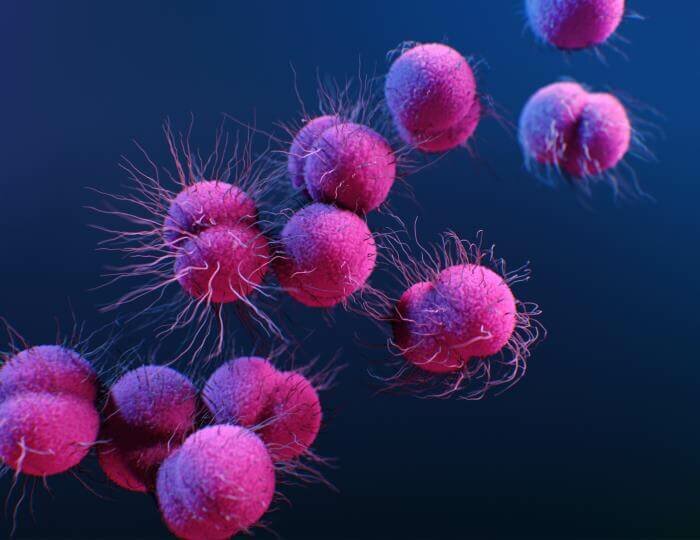
Introducing Neisseria gonorrhoeae
Neisseria gonorrhoeae (nice-ear-rea gone-oh-rea), the bacterial cause of gonorrhoea, a sexually transmitted infection or STI, was discovered in 1879 by a German doctor, Albert Neisser.
Gonorrhoea has been known by the pseudonym, the Clap, which is much easier to pronounce and spell! N. gonorrhoeae also goes by other aliases, such as NG, gonococcus (singular), gonococci (plural) or GC for short.
In 2020, the WHO estimated that there were over 82 million new cases of gonorrhoea worldwide. What does 82 million people look like? Almost the entire population of Germany (n = 84,566,382).
Neisseria gonorrhoeae: the successful pathogen
N. gonorrhoeae has existed alongside humans for a long time; there are reports that describe symptoms matching those of gonorrhoea dating from 130 AD (Vicentini et al., 2019).
One characteristic of gonococci that make them a particularly stealthy pathogen is their ability to survive in the human body without causing symptoms. More than 50% women with endocervical infection will be asymptomatic, although most men (~90%) will experience symptoms (Unemo et al., 2020).
A common symptom of anogenital gonorrhoea is a purulent urethral or vaginal discharge; however, other symptoms include vaginal pruritis, cervicitis, vulvovaginitis, vaginosis, salpingitis, lower abdominal pain, and pelvic inflammatory disease (women) and prostatitis and epididymitis (men).
Other STIs, such as chlamydia, Mycoplasma genitalium, and trichomoniasis, may present with similar symptoms, or be carried asymptomatically. Additionally, coinfection with one or more STI-causing organisms is common. Accurate diagnosis is essential as each infection requires different treatment.
In this situation, syndromic testing (the simultaneous detection and differentiation of multiple pathogens that cause similar symptoms) for gonorrhoea, chlamydia, M. genitalium, and trichomoniasis offers a practical solution.
If implemented directly at the point of need, syndromic testing enables healthcare professionals to make informed decisions about appropriate antimicrobial treatment during a patient consultation rather than offering empirical treatment while waiting for the results of centralised laboratory testing.
Neisseria gonorrhoeae: the immune system evader
Another characteristic that contributes to the success of N. gonorrhoeae is the ability to evade the immune system and cause reinfection.
A protective immune response relies on the body recognising previously encountered pathogens. N. gonorrhoeae, however, changes the proteins present on the surface of its cells, enabling the pathogen, on a subsequent encounter with the immune system, to go unrecognised.
As a result of this phenomenon, known as antigenic variation, the immune system cannot protect against subsequent infection and reinfection is possible after re-exposure. The variability of cell surface proteins and lack of immune response is also one reason why there is no vaccine against N. gonorrhoeae.
With no help from the immune system and no vaccine, we rely on antibiotics for curative treatment and control of spread. Currently, first-line antibiotic treatment for uncomplicated anogenital gonorrhoea is a single dose of intramuscular ceftriaxone (UK, USA) either with or without a single oral dose of azithromycin (Europe).
Neisseria gonorrhoeae: acquires antibiotic resistance genes
N. gonorrhoeae have another survival trait to keep them one step ahead of antibiotics.
Gonococci have an innate ability to pick up pieces of ‘free’ DNA i.e., those not encased within a cell. This ability, known as being genetically competent, is not something that N. gonorrhoeae ‘thinks’ about, rather they act like a vacuum cleaner and take up free extracellular DNA.
Unlike other genetically competent bacteria, gonococci do not regulate this process, meaning that the ability to pick up DNA is switched on throughout the lifecycle of the cell.
If these pieces of DNA comprise antibiotic resistance genes, the genes may become incorporated into the bacterial chromosome or onto mobile plasmids (circular pieces of DNA that can be transferred between bacteria) of N. gonorrhoeae. When this occurs, the bacteria are described as having acquired antibiotic resistance.
The implications of drug-resistant gonorrhoea
If antibiotics are the last line of defence against N. gonorrhoeae, what happens when the bacteria develop antimicrobial resistance (AMR) or have reduced susceptibility to an antibiotic?
Typically, N. gonorrhoeae responds well to antibiotic treatment if the bacteria are susceptible; however, when gonococci have reduced susceptibility to an antibiotic it means there is a reduced likelihood that the infection will respond to treatment with that antibiotic.
Given that most treatment for STIs is empirical (best guess), if N. gonorrhoeae has reduced susceptibility to the antibiotic prescribed there is a risk of prolonged infection and continued exposure of sexual contacts.
Neisseria gonorrhoeae: the journey to multi-drug resistance
N. gonorrhoeae reached ‘superbug’ status in the US in 2007 (Unemo et al., 2020). ‘Superbug’ is a colloquial term that is used to describe a microorganism that has developed resistance to different antimicrobial drugs.
The first high-level ceftriaxone-resistant (2mg/L) strain (H041) was detected in Japan in 2009 and reported in 2011. Other ceftriaxone-resistant strains of N. gonorrhoeae have been identified in Australia, Austria, France, and the UK.
The latest reports of multi-drug resistant N. gonorrhoeae from the USA are further examples of N. gonorrhoeae that have developed resistance or are no longer susceptible to treatment with five different classes of antibiotics.
Neisseria gonorrhoeae: harnessing point-of-care testing for effective diagnosis
Spread of multi-drug resistant N. gonorrhoeae, especially those strains with reduced susceptibility to ceftriaxone and high-level resistance to azithromycin, are of significant public health concern due to the limited available options for treatment.
Besides the risk of onward transmission to sexual contacts, if left untreated gonococcal infection can cause a range of secondary complications. These include pelvic inflammatory disease, male and female infertility, complications in pregnancy and poor foetal outcome, and enhanced susceptibility to infection with HIV (WHO).
Detection of multiple pathogens and any associated drug resistance markers in a single test offers an opportunity to ‘treat right first time’. Syndromic testing that includes well characterised antimicrobial resistance markers for N. gonorrhoeae (and M. genitalium which is also associated with multiple drug resistance) at the point-of-need offers significant advantages in terms of patients lost to follow up.
In addition to the convenience and reassurance for the patient, other benefits include fewer clinic attendances, reduced onward transmission events and fewer instances of presumptive treatment for asymptomatic sexual contacts.
Rapid point-of-need tests indicating susceptibility to second line treatment options, such as ciprofloxacin, could identify patients with gonococcal infections that may respond to alternative antibiotics to reduce the overuse of first line ceftriaxone as an empirical treatment, thus preserving its effectiveness for longer.
Neisseria gonorrhoeae: the future
So far, cases of multi-drug resistant N. gonorrhoeae have responded to antibiotic treatment, either by using a higher dose of an antibiotic or using antibiotics that are only available as an intravenous option.
While novel drugs to treat gonorrhoea are part of the solution to “stop untreatable gonorrhoea becoming a reality in the near future” (Day et al., 2022), history would predict it is highly likely that resistance could develop to these new agents over time.
Currently, the global extent of resistance in N. gonorrhoeae is largely unknown due to limited testing opportunities and availability of robust surveillance data in many regions (WHO). Improving access to convenient testing is vital to enable prompt, tailored treatment and rapid testing of sexual contacts.
Whatever it takes, systematic global action against multi-drug resistant N. gonorrhoeae is urgently needed.